Healthcare / New models of care
Adopting the Scandinavian Sengetun model to design for end-of-life care
By Alastair Forbes and Oliver Jones | 10 Oct 2019 | 0
This poster presents the research-informed practice and client collaboration we delivered to build a 21st-century palliative care facility, using a Scandinavian model of care for the first-time ever in the UK.
Abstract
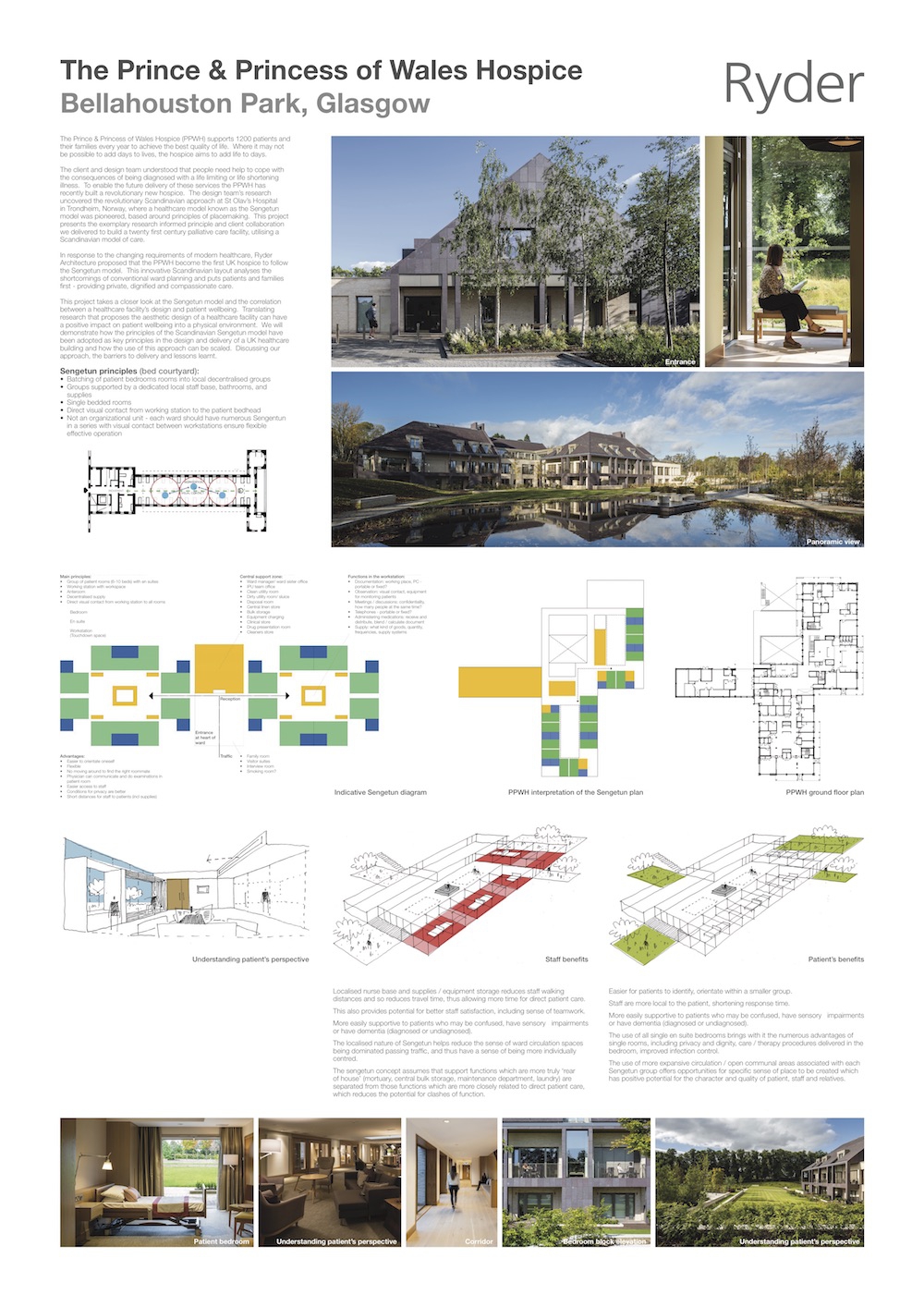
The Prince & Princess of Wales Hospice (PPWH) supports 1200 patients and their families every year to achieve the best quality of life. Where it may not be possible to add days to lives, PPWH aims to add life to days. The client and design team understood that people need help to cope with the consequences of being diagnosed with a life-limiting or life-shortening illness. To enable the future delivery of these services, the PPWH has recently built a revolutionary new hospice. The design team’s research uncovered the revolutionary Scandinavian approach at St Olav’s Hospital in Trondheim, Norway, where a healthcare approach known as the Sengetun model was pioneered, based around principles of ‘placemaking’.
This poster presents the research-informed practice and client collaboration we delivered to build a 21st-century palliative care facility, using a Scandinavian model of care for the first-time ever in the UK.
This innovative Scandinavian layout analyses the shortcomings of conventional ward planning and puts patients and families first – providing private, dignified and compassionate care. This poster takes a closer look at the Sengetun model and the correlation between a healthcare facility’s design and patient wellbeing. Translating research that proposes the aesthetic design of a healthcare facility can have a positive impact on patient wellbeing into a physical environment. We’ll demonstrate how the principles of the Scandinavian Sengetun model have been adopted for the first time as key principles in the design and delivery of a UK healthcare building, and how the use of this approach can be scaled.
The facility offers patients the quality of life they deserve in a place like home while the clinical and medical assistance is covert, and takes advantage of assistive technologies where possible. This makes it easier for patients to identify and orientate themselves comfortably within smaller groups, as well as shortening staff response times to improve patient safety and support.
The design approach and resulting building has proven to be especially supportive to patients with confusion, sensory impairments or dementia. The measures adopted resulted in open communal areas that offer opportunities to create a sense of place, adding to the character and quality of all visitor experiences. Staff walking distances and travel times are reduced, allowing more time for direct patient care, and higher levels of staff satisfaction and better collaboration.
New assistive technologies were embraced and contribute to the changing landscape of care delivery. The nurse’s station uses wireless technologies, freeing staff from static observation stations, and improving visual links and patient proximity. The scheme is now acting as a testbed with a number of ongoing research projects underway, to gather evidence and inform the future design of health facilities.
Organisations involved